Ultrasound is likely to play a great role in managing patients with COVID-19 infections, given that it can be done at bedside avoiding transportation, and exposing additional staff members.
Key Points
- No need to transport or expose additional staff to potential infected individuals
- SARS-CoV-2 is sensitive to most standard viricidal disinfectant solutions but care must be taken when cleaning (whole ultrasound machine, cords, probes, etc) 4
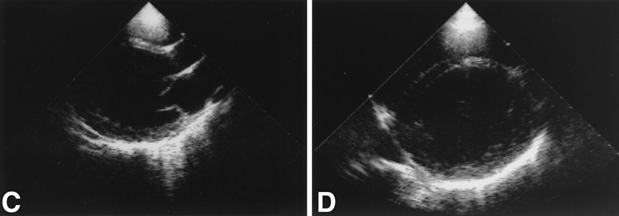
- Cases of myocarditis have been reported in hemodynamically unstable patients with COVID-19 with POCUS showing markedly decreased global left ventricular systolic function (IMAGE 1)2,12
- Lung ultrasound has shown irregular pleural lines with small subpleural consolidations, areas of white lung with irregular vertical artifacts (B-lines), and alveolar consolidation as evidenced by dynamic/static air bronchograms on pulmonary exam (IMAGE 2)5,14
Point of care ultrasound has been used to aid in the diagnosis and management of patients with COVID-19.5 It is readily available in most intensive care units and its use requires no patient transportation or additional staff exposure.
Ultrasound machines require cleaning and sterilization after each use to prevent spread to patients and other healthcare workers, with some institutions using disposable plastic covers while others set aside certain machines for COVID-19 patients.4 SARS-CoV-2 is sensitive to most standard viricidal disinfectant solutions, though wet times vary (Sani wipes 2 minutes, Oxivir wipes 1 minute).12 Care must be taken to clean the entire machine (probes, cords, screens, etc) and ultrasounds should be cleaned in the patient’s room/antechamber and once again in a hallway.4 This makes smaller, tablet/phone ultrasounds more appealing for ease of cleaning, though need for image quality should be determined before entering a room.4 Sterile, single-use gel packets are preferable to nonsterile gel when possible infection is a concern.3
There have been case reports of myocarditis associated with COVID-19, though no direct visualization of viral infiltration of myocardium has been observed on electron microscopy. 2 As such, assessment of cardiac function is reasonable in patients with hemodynamic compromise.2 Patients that have presented with myocarditis have experienced hemodynamic instability with ST segment elevations, elevated BNP/troponin, normal coronary anatomy imaging, and markedly decreased global left ventricular systolic function (IMAGE 1).2,12
On pulmonary exam, cases reports have shown irregular pleural lines with small subpleural consolidations, areas of white lung with irregular vertical artifacts (B-lines), and alveolar consolidation as evidenced by dynamic/static air bronchograms on pulmonary exam (IMAGE 2).5,14 In the resolution of the disease, reappearance of A-lines can be seen.14 Given the nonspecific nature of these findings there is inadequate data to suggest the use of lung ultrasound as a diagnostic tool for COVID-19.

References
- Ai T, Yang Z, Hou H, et al. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020:200642.
- Cardiology ACo. Cardiologist’s Insights From Treating COVID-19 Patients in China. American College of Cardiology. ACC News Story Web site. Published 2020. Accessed 3/12/2020, 2020.
- Medicine AIoUi. Guidelines for Cleaning and Preparing External- and Internal-Use Ultrasound Transducers Between Patients & Safe Handling and Use of Ultrasound Coupling Gel. American Institute of Ultrasound in Medicine. Published 2018. Accessed 05/16/2017, 2017.
- Echocardiography ASo. ASE Statement on COVID-19. American Society of Echocardiography. Published 2020. Accessed2020.
- Buonsenso D, Piano A, Raffaelli F, Bonadia N, de Gaetano Donati K, Franceschi F. Point-of-Care Lung Ultrasound findings in novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24(5):2776-2780.
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507-513.
- Chung M, Bernheim A, Mei X, et al. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology. 2020;295(1):202-207.
- Fang Y, Zhang H, Xie J, et al. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020:200432.
- Felker GM, Boehmer JP, Hruban RH, et al. Echocardiographic findings in fulminant and acute myocarditis. J Am Coll Cardiol. 2000;36(1):227-232.
- Kanne JP, Little BP, Chung JH, Elicker BM, Ketai LH. Essentials for Radiologists on COVID-19: An Update-. Radiology. 2020:200527.
- Kenny J-E, Canepa C. An Illustrated Guide to the Chest CT in COVID-19. PulmCCM. Published 2020. Accessed2020.
- COVID-19 Preparedness for Echo Labs: Insights from the Frontlines. Youtube: American Society of Echocardiography; 2020.
- Ling Z, Xu X, Gan Q, et al. Asymptomatic SARS-CoV-2 infected patients with persistent negative CT findings. Eur J Radiol. 2020;126:108956.
- Murphy A, Bell D. COVID-19. Radiopaedia. Published 2020. Accessed2020.
- JCL R, Hare S, Edey A, et al. An update on COVID-19 for the radiologist – A British society of Thoracic Imaging statement. In. Clinical Radiology: Elsevier; 2020.
David Gordon, MD